The Link Between Macrophage Senescence and Blood Vessel Formation
Recent research published in Aging Cell has unveiled a fascinating connection between macrophage senescence and impaired blood vessel formation. This impairment could be a pivotal factor in the onset of peripheral arterial disease (PAD), which affects over 113 million people globally. The concerns surrounding PAD are heightened when we consider that surgical interventions among older patients can carry significant risks, sparking interest in non-invasive regenerative treatment options.
Understanding the Role of Macrophages in Angiogenesis
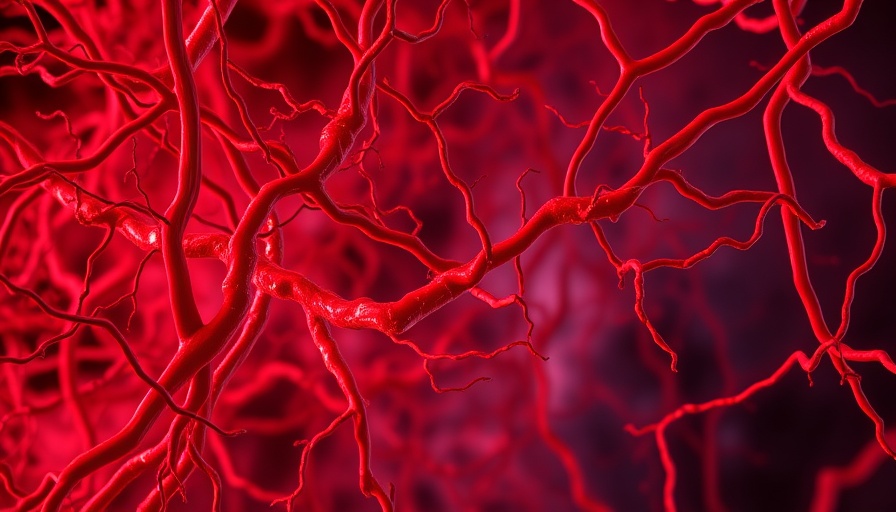
Macrophages, the body’s immune response cells, typically promote angiogenesis—the process of new blood vessel formation. However, as these cells age, they undergo senescence—a state associated with increased inflammatory factors and decreased proliferative capabilities. This leads to a pronounced shift in the production of vascular endothelial growth factor A (VEGF-A), specifically a decrease in the beneficial isoform, VEGF-A165A, and an increase in the antagonistic form, VEGF-A165B. This crucial change can severely hinder the angiogenic potential of endothelial cells, further exacerbating conditions like PAD.
Experimental Insights: Testing Macrophages on Young Mice
The study conducted by researchers involved various experimental setups, one of which tested the impact of senescent macrophages on young mice after an induced hindlimb injury. Results revealed stark differences; while young, healthy macrophages had no negative impact, senescent macrophages led to alarming complications, including increased tissue necrosis and reduced capillary formation. Such outcomes underline the detrimental effects of macrophage senescence on blood flow and tissue regeneration, marking a significant area of concern for treating age-related blood vessel diseases.
Unraveling the Mechanism: How VEGF-A165B Impairs Healing
The relationship between senescent macrophages and endothelial cell function was further elucidated. By manipulating macrophage production of VEGF-A165B—either by knocking down the gene responsible or via the introduction of a specific antibody—the researchers were able to mitigate the damaging effects observed on endothelial cells. Both interventions effectively enhanced angiogenesis, signaling a promising route for therapeutic development directed at macrophage senescence.
Implications for Future Treatment Strategies
This emerging evidence presents an opportunity for novel therapeutic strategies aimed at addressing PAD and other ischemic conditions. By targeting VEGF-A165B in senescent macrophages, scientists may pave the way for treatment modalities that enhance the body's capacity for self-repair by promoting healthy blood vessel formation. The implications for patient quality of life could be profound, particularly in an aging population increasingly affected by vascular complications.
Conclusion: A Perspective on Longevity and Vascular Health
As the understanding of macrophage behavior evolves, so does potential for treating age-related health issues. The findings from this study not only contribute to the science of aging and vascular health but also encourage ongoing dialogue on how best to manage and treat conditions that affect significant portions of the population. This is a moment for both scientific and public health perspectives to collaborate, advocating for research that directly translates into meaningful health improvements.
 Add Row
Add Row  Add
Add 




Write A Comment